Author: James Organ | Posted On: 23 Jan 2026
Access pressures in Australia’s healthcare system are most visible among people living with chronic illness. Using a narrower definition of selected chronic conditions, including common and clinically significant diseases, ABS National Health Survey; AIHW Chronic Conditions report around 12.6 million Australians, approximately 50% of the population, were living with at least one chronic conditions according to national health data.
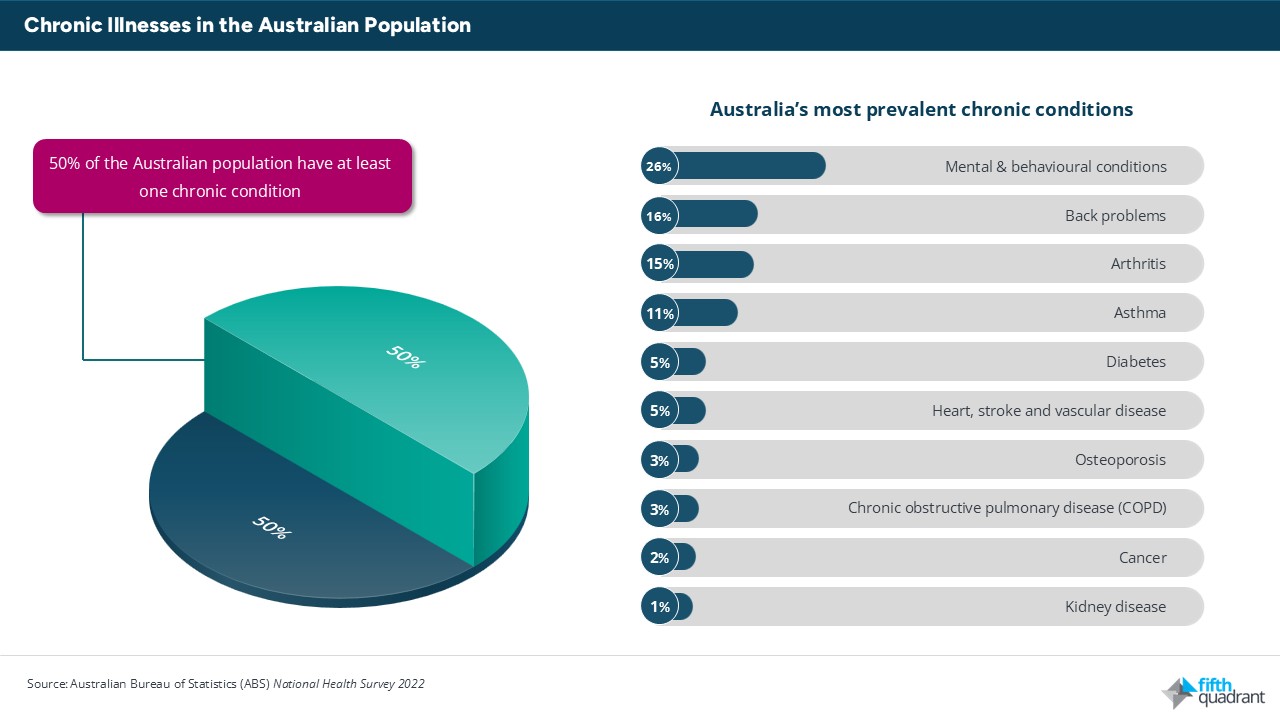
This prevalence means chronic illness is not confined to a small or marginal segment of the population. It affects Australians across age groups, income levels, and geographies, and is a defining feature of demand for primary healthcare services.
These individuals account for a substantial share of primary care usage. Chronic conditions typically require:
- Interactions with allied health and specialist services
- Ongoing GP visits
- Regular monitoring
- Prescriptions
- Referrals
As a result, access to affordable and continuous care is a practical issue rather than an occasional one, particularly for people managing multiple conditions or complex care needs.
Cost, Medicare, and ongoing care
For people with chronic illness, healthcare costs are cumulative. While individual out-of-pocket costs for a single consultation may appear manageable, the frequency of care means total annual expenses can become significant over time. This is especially relevant for patients requiring regular reviews, diagnostic testing, and medication management.
Working-age adults face particular challenges. This group is less likely to be bulk billed consistently and may not qualify for concession-based eligibility. As a result, affordability can become a constraint on access, even where clinical need is ongoing.
Medicare provides specific mechanisms to support chronic disease management, including chronic disease management plans and team care arrangements. These allow for structured GP involvement and limited subsidised access to allied health services. However, funding remains tied to individual services and encounters, rather than to longitudinal care pathways or patient outcomes. This shapes how care is delivered in practice, particularly in high-demand settings.
Workforce, geography, and care delivery
Workforce availability plays a critical role in determining access to care for people with chronic illness. Regions with higher prevalence of chronic conditions often overlap with areas experiencing GP and allied health shortages. This can limit appointment availability, disrupt continuity of care, and increase reliance on incentive-based bulk billing arrangements.
Geographic variation in access remains a consistent feature of the system. Patients in regional and outer metropolitan areas may face longer wait times, fewer provider options, and greater reliance on a small number of practices. These factors compound access challenges for people who require frequent or ongoing care.
Role of digital and team-based care
Digital health tools, telehealth, and team-based models are increasingly used to support chronic disease management, particularly where in-person access is constrained. The Australian Institute of Health & Welfare shows that digital health can facilitate routine follow-ups, medication reviews, and monitoring, reducing the need for travel and improving continuity for some patients.
Team-based models, incorporating nurses and allied health professionals, can also play a role in managing demand and supporting coordinated care. However, adoption varies across practices and regions and depends on workforce capacity, funding arrangements, and digital infrastructure. These approaches are often additive rather than substitutive, supplementing traditional care rather than replacing it.
Conclusion
The scale of chronic illness, affecting around half of Australians, has direct implications for healthcare utilisation, access to care, and Medicare-funded primary care services. Patterns of bulk billing, workforce distribution, and funding design all influence how effectively ongoing care is delivered to this group.
At Fifth Quadrant, we specialise in healthcare market research that delivers deep insights into patient needs, provider challenges, and system-level barriers. Our research helps healthcare organisations, policymakers, and innovators design better services, improve access, and deliver more effective care. Contact us to learn how our insights can support your healthcare strategy.
Posted in Uncategorized, Healthcare, TL

